Welcome to Hitting the Books. With less than one in five Americans reading just for fun these days, we've done the hard work for you by scouring the internet for the most interesting, thought provoking books on science and technology we can find and delivering an easily digestible nugget of their stories.
The Angel and the Assassin: The Tiny Brain Cell That Changed the Course of Medicine
by Donna Jackson Nakazawa

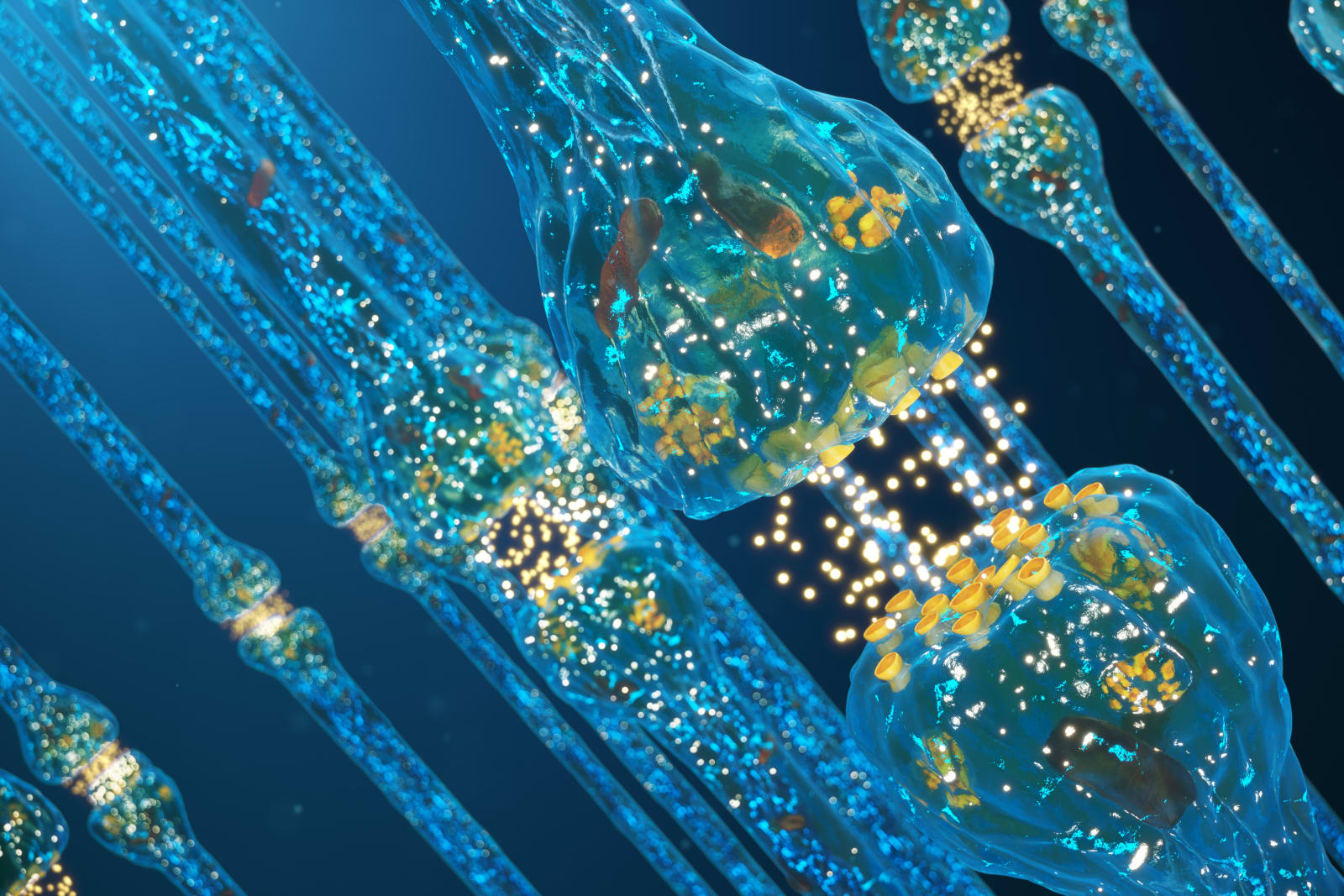
Whether you've just gotten your bell rung, your clock cleaned, or are simply seeing stars -- congratulations, you're likely concussed. When that happens, microglial cells, the human brain's first line of immune defense, will set about eating dead and damaged neurons from the injured site before returning to their normal duties of clearing amyloid plaques. But suffer a lifetime of blows to the head, as many National Football League players do, and those microglia might not revert back to their tame housekeeping roles after pruning your prefrontal cortex. Instead, they could continually devour injured and healthy neurons alike, resulting in symptoms that appear eerily similar to CTBI.
But microglia aren't all bad, or even a little. As author Donna Jackson Nakazawa illustrates in her fascinating book, The Angel and the Assassin, these otherwise unobtrusive brain cells could hold the key to our better understanding a wide range of human neurological and autoimmune issues.
So how can it be that a blow to the head can wreak such havoc to the nimble workings of the mind, and continue to do so year after year, long after the injury has occurred?
Researchers have known for some time, based on autopsies of the brains of individuals who suffered traumatic brain injury and who died years later from other causes, that these brains showed an unusual level of microglial activity. But this frenzy of agitated microglia was not seen, says [former Chief of Neurology at the VA Medical Center in San Francisco, Dr. Alan] Faden, as an important factor in progressive brain damage.
Faden and his team began looking more closely. Using MRI imaging, they examined the brains of mice who'd been exposed to moderate traumatic brain injuries and found that microglia remained over-excited for up to a year following the original injury. These mice also showed neurodegeneration in the brain's hippocampus, and their biomarkers for neuroinflammation were significantly higher than normal.
"We wondered what part microglia were playing in this and found, to our great surprise, that they were taking on myriad roles. We could distinguish many different populations of microglial cells," he explains. "The microglia weren't just either good or bad, yin or yang. There were many different subsets with different neurotoxic capacities." Many of which caused mayhem in the brain.
And once researchers like Faden began to take these newly understood immune cells in the brain into account, the field's understanding of concussion catapulted forward.
Faden's investigation into microglia's role in concussion took place just a few years after Beth Stevens did her groundbreaking work at Harvard showing that some triggered microglia were eating synapses, while others were spewing out inflammatory cocktails that caused neuroinflammation.
Faden now believes that the activation of toxic microglia is the major contributor to chronic traumatic brain inflammation, and the associated brain cell loss and brain dysfunction that is the hallmark of CTBI. An injury to the head triggers microglia to switch from protecting and repairing the brain to excreting inflammatory chemicals that create more microglia-driven runaway inflammation. When this happens, activated microglia increase in size, becoming big and bulky and bushy; they look like loping tarantulas under the microscope. They bite away at synapses, leading to loss of memory, concentration, clarity of mind, and buoyancy of mood.
Once these microglia forest fires get going, without intervention, they become harder and harder to put out, and CTBI can develop.
But because scientists missed, for so long, the fact that microglia could become chronically active and destructive after head injury, clinicians weren't making this crucial connection and utilizing it to improve patient treatment—not by a long shot. For instance, if a boy was knocked out cold by a soccer ball in middle school and then developed depression or a panic disorder or struggled academically in high school, the link between his earlier head injury and later learning issues and depression flew completely under the radar.
Which leads us to Faden's most recent -- and, to my mind, most surprising -- discovery. In 2017, Faden found in animal studies that those with a traumatic brain injury had higher levels of unique microparticles in the blood, as compared to other animals. When Faden traced where those particles originated, he found that they were being directly released by microglia. After an injury, the response of microglia was so out of proportion that microglia were driving these microparticles into other areas of the brain, far from the site of the original injury, stoking up more inflammation, leading to more tissue damage. Astonishingly, some of these particles that microglia projected forth were getting released right into the body's bloodstream.
And, as scary as it sounds, his knowledge is very helpful and promising news.
Remember Beth Stevens's hope that we will soon possess clear blood biomarkers to accurately measure factors that microglia secrete as they begin to shift from angels to assassins, so that we can better grasp what microglia are doing in the brain, in terms of denuding synapses, through simple blood tests?
Once these microglia-derived microparticles can be accurately measured by a common blood test, these biomarkers can be used to monitor concussion treatment and healing. Imagine, for instance, that a woman has a mild head trauma in a car accident. Clinicians may one day be able to test her blood to see how much inflammation is brewing in her brain and how severe her concussion is, and then continue to run routine blood tests to evaluate how well she's responding to treatment. If lab tests show she still has high levels of microglia-driven inflammatory microparticles in her blood, she will need further treatment and observation. If levels of microglia microparticles rapidly decline, practitioners will know she's well on the road to healing.
Faden's lab has revealed one other remarkable finding. Traditionally, he says, research on spinal cord injuries has neglected the effects of those injuries on brain function. But spinal cord injuries, he says, can cause widespread and sustained brain inflammation, progressive loss of brain cells, cognitive decline, and depressive symptoms—by provoking microglia to create invisible havoc in the brain.
This bidirectional chatter between the central nervous system's immune response (via the cerebrospinal fluid, intersecting with the lymphatic pathways that run through the meningeal spaces of the brain) and microglia makes it even clearer that brain and body are in constant conversation.
For instance, in one 2017 study, Swedish epidemiologists at the Karolinska Institute scoured eighty thousand adult health records and reported that teens who'd experienced a single concussion were 22 percent more likely to later develop multiple sclerosis, compared to those who'd never had a head trauma—and for those with multiple concussions, the increased risk of developing MS rose to 150 percent. At this point, given what we know about the feedback loop between body and brain -- and the way in which microglial cells in our brain and the immune cells in our body chit-chat -- this is hardly surprising.
So let's pause for a moment and acknowledge that all of this new information about head injury and concussion is pretty frightening. It certainly scares me. In addition to my autoimmune issues, I've had two mild concussions. Twenty-five years ago my husband and I were going to the movies. When we got to the movie theater, I dashed out of the car to buy the tickets while he parked. My purse strap had become wrapped around the stick shift, and as he pulled away, my head ricocheted back, hitting the roof of the car. Back then, they called it a brain bruise. The second time, sixteen years ago, I was a passenger in a car driven by a friend. She hit a patch of black ice while we were going down a hill and we hit a telephone pole—and I struck my head on the passenger side window. I rested, iced, recovered, little by little. But it makes me wonder. The same year that I had that second concussion in the car accident, I later developed Guillain-Barré syndrome—a disease similar in pathogenesis to multiple sclerosis—for the first time. Might there have been some connection? It is impossible to say. But clearly, the idea that chronic traumatic brain inflammation may be occurring and causing unsuspected mental and physical havoc is dismaying for any individual, or parent of a child, who's had a head injury.
I tell Faden that I'm afraid that all this information is going to be very scary for readers—they'll want to throw this book right out the window."I imagine it does sound frightening," he says. But then his face brightens. "The most important message, though, is this. Although CTE is not a treatable disease, mild and moderate concussion are on the cusp of becoming very treatable." As he talks, he gently punches the first two fingers of his left hand into the air with excitement. For decades Faden has been working to develop anti-inflammatories that have the potential to ameliorate and reverse brain injury, alongside other interventions -- and he feels that new approaches may be able to limit bad outcomes after concussive brain injuries.
Over the course of his career -- long before there was an understanding of the role that microglia play in concussion—Faden and his colleagues went through a cycle of hope and frustration, introducing an array of different drug treatments into the bloodstream—including selected anticancer drugs, thyrotropin-releasing prolactin (or TRH), and glutamate-blocking drugs. Delivered within a few minutes, hours, or, in some cases, days of injury, these varied therapies dramatically reduced the level of neurotoxicity and cell death after a head injury.
But the problem has been, Faden says, resting his palm in his cheek for a moment as he continues, that because some of these agents were no longer subject to patent restrictions, pharmaceutical companies weren't interested in investing in them. There was no money to be made. Unfortunately, says Faden, "Despite the fact that these medications show exceptional promise experimentally, they will never be examined in large clinical trials."
So what new treatments are on the horizon? Once again, it all comes down to the promise and peril of microglia.
Faden has found that by using a combination of newly studied and non-invasive approaches, physicians can help patients tamp down overexcited microglia, even weeks or months after a mild or moderate brain injury has occurred—making it possible to intervene to help a far wider swath of patients more of the time.
Right now, Faden's lab is studying the effects of combining "three simple and easily available approaches," he explains. "These include aerobic exercise, dietary manipulations such as intermittent fasting, and computer brain training."
UCLA researchers recently found that exercise -- done within certain windows of time after a concussion and only with a doctor's approval -- increases chemical factors in the brain that damp down the hyperactivity of microglia. Faden's lab is also the first to investigate whether an intermittent fasting diet—in which patients fast for long stretches in between normal eating—will increase protective brain factors when done in conjunction with aerobic exercise. (Animal studies on intermittent fasting after traumatic brain injury have been promising.) He hopes that when they also add in computer brain training to improve cognitive function, alongside exercise and dietary changes, they will see added benefits.* Right now he and his colleagues are testing this simple triad of ideas on mice, but they plan to conduct human trials in the future.
Together, these new investigations will give us far more insight into how, says Faden, "we can potentially intervene months or even years after an injury, offering novel treatments long after the initiating insult."
Faden and others are now experimenting with delivering a new microglia-targeted treatment that can eliminate almost all microglia -- both the good guys and the bad guys. After treatment, newborn microglia begin to repopulate the brain, and as they do, they become neuroprotective rather than neurotoxic. The big bad assassin microglia are no longer on the scene; only the angels are perusing the brain. One month later, "the toxic population of inflammatory microglial cells is still markedly reduced," Faden, says, his voice full of excitement.
It's a little like rebooting your computer -- hitting the coding keys to delete everything and rebuilding your operating system over again without the computer viruses or glitches.
This oral anti-inflammatory medication -- what we might think of as a kind of fire extinguisher for the brain -- is still several years away from clinical trials, let alone being available to patients, but it adds to the sense of hope on the horizon for patients with concussions and brain injuries.*
"If we can change the level of microglia-driven inflammation through these multiple interventions simultaneously, we should be able to change patients' outcomes after brain injury," says Faden. "We are getting so much closer."
----
* Of course, like all new drug therapies, this treatment will need to go through extensive clinical trials that will have to be replicated and repeated in order to evaluate efficacy, safety, and potential side effects.
* Patients with concussion or head injury should always consult their physician or concussion specialist for advice about when and if it's appropriate, in their particular case, to consider exercise, a fasting diet, brain training, or neurofeedback. None of these therapies should be undertaken other than at a physician's suggestion and under his or her supervision.
From The Angel and the Assassin: The Tiny Brain Cell that Changed the Course of Medicine by Donna Jackson Nakazawa published on January 21, 2020 by Ballantine Books, an imprint of Penguin Publishing Group, a division of Penguin Random House LLC. Copyright © 2020 Donna Jackson Nakazawa.
via engadget.com



0 Response to "Hitting the Books: These brain cells could hold clues to the CTBI crisis"
Post a Comment